Vitreo-Retinal Services

Vitreous Bleeds
Vitreous is the name of the deep-seated, clear, gel-like substance found inside the eyeball which is responsible for maintaining the shape of the eye. Vitreous bleeds or hemorrhages are actually a misnomer as it is not the vitreous that bleeds (as the vitreous itself has no blood vessels), but rather the retinal vessels that bleed into the vitreous.
Vitreous hemorrhage or bleeding inside the eye is a serious condition that may occur due to trauma or due to certain diseases of the eye like Diabetic Retinopathy or Eale’s disease. Bleeding may be minor leading to complaints of a ‘shower of particles’ in the visual field especially on movement. Or it may be major leading to loss of vision. Bleeds may subside on their own with small amounts of blood getting naturally reabsorbed. Larger bleeds may require surgical intervention called a vitrectomy to re-establish vision. Many times exact cause can only be established after vitrectomy. Bleeds may recur depending on the cause. In all circumstances, the situation merits careful examination and assessment of the underlying cause and its treatment. Vitreous which is removed is replaced by air, other gases, fluid, or oil depending on the cause. Multiple surgeries may be required.
Retinal Detachment
Retina is the innermost light-sensitive layer of the eye which converts the light entering the eye and focusing upon it, into electrical impulses that are sent to the brain via the optic nerve. There, these impulses are interpreted as an image.
Retinal detachment, as the name suggests, is said to occur if the retina detaches from other layers of the eye.
Patients complain of sudden painless loss of vision which may affect a part or the whole of the visual field. This may progress from partial to complete loss of vision if not treated. In very severe cases, not only vision but even the shape of the eye can be affected.
There are 3 main types of retinal detachments (RDs):
- Tractional– due to traction of the vitreous on the retina- often seen in diabetic retinopathy
- Rhegmatogenous– due to tears in the retina which may occur in trauma, high myopes, or degenerative conditions of the retina. Here fluid may seep under the tear leading to a detachment
- Exudative– due to the presence of inflammation or a tumor
The treatment of RDs is most often surgical and needs to be done at the earliest to get the best possible visual results. For as long as the retina is detached, its circulation and nutrition are compromised, so the longer the duration of the detachment, the poorer the visual result. By various techniques, the retina is replaced in its original position and then held there. The patient may need to maintain a certain position for some time after the surgery. Many times more than one surgery may be required especially if oil is injected in the eye.
Medical Retina
Not all vitreo-retinal conditions require surgical intervention. Some are managed totally by medical means in the form of eye drops, tablets, and injections. Macular Degeneration, CRVO, BRVO, and optic neuritis are examples of diseases that come under the purview of the medical retina.
Macular Degeneration (ARMD)
Age-related macular degeneration is a condition seen in older persons that results in painless loss of central vision. This may be quite debilitating as the macula (area of sharpest vision) is primarily affected. Assessment and progression are done by non-invasive OCT. Many patients benefit from intra-ocular injections of certain medications.
Endophthalmitis
As suggested by the name, endophthalmitis means infection inside the eye. This is a vision threatening condition which may occur due to trauma to the eye, intra-ocular foreign bodies and very rarely after surgery to the eye. On occasion it may also occur without surgery, by transfer via blood from another source of infection in the body (Endogenous).
Under normal conditions, the inside of the eye is sterile and clear so that light may enter the eye and the person sees. Infection inside the eye results in a strong bodily response as occurs anywhere else in the body. But invasion by infection fighting cells, growth of blood vessels, swelling and collection of debris inside the eye produces devastating effects on vision by not only causing opacification of transparent areas but also by adversely affecting the metabolism of numerous delicate structures inside the eye especially retina and optic nerve
In early and mild to moderate cases, antibiotics , especially intravitreal, may be used. In more severe cases surgery may be required to remove the infection from inside the eye by doing pars plana vitrectomy and reestablish a clear medium through which sight may be restored.
Macular Degeneration
Although a leading cause of blindness in people 60 and older there are measures that can be taken to slow progression of the condition and newer treatments can help reduce irreversible blindness.
What is age-related macular degeneration?
Age-related macular degeneration (AMD) is an eye condition that causes painless loss of central vision and is most common in people over the age of 50. AMD currently is one of the leading cause of vision loss in the developed world. It is estimated that at least 1 in 10 people over the age of 65 have some signs of AMD and that its incidence will continue to increase due to longer life expectancy and dietary changes.
What are the signs of AMD?
Early symptoms of AMD may include difficulty in reading, difficulty in recognizing people’s faces and distortions in the central vision. The sight loss usually occurs gradually over time, although it can develop very rapidly due to sudden bleeding in the central area of the retina, the macula, with loss of central vision within a few days.
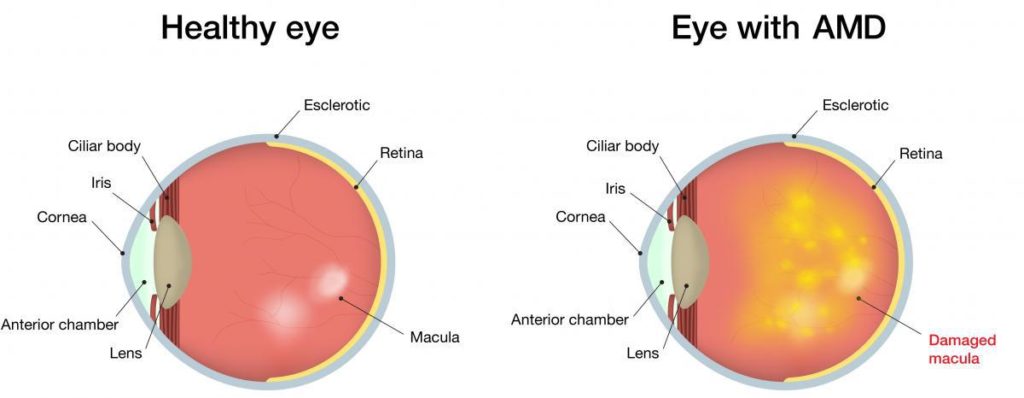
Dry AMD and Wet AMD
Dry AMD is the most common, but less serious form of the disease affecting about 85% of patients. The cones and rods photo-receptors in the central retina become damaged and the central vision progressively deteriorates very slowly over a number of years.
Wet AMD is the most serious type affecting approximately 15% of patients and it is so called because abnormal new vessels grow under the retina and result in leakage of fluid and blood in the macula with rapid loss of central vision within days. This condition can now be successfully slowed down by early intervention in order to prevent permanent loss of central vision.
What are the treatments for wet AMD?
The treatment of wet AMD has been transformed over the past few years by the drugs which block the vascular endothelial growth factor (anti-VEGF) including Eylea (Aflibercept), Lucentis (Ranibizumab) and Avastin (Bevacizumab). These treatments are given as injections directly into the eye (intravitreal injections) under local anaesthetic at around 4 to 8 weekly intervals and are effective at slowing down AMD progression, preserving eyesight and limiting permanent damage on the macula.
“We are extremely lucky to be able to offer these new treatments for AMD, however the early detection of wet AMD always results in better preservation of sight and reduces the risk of permanent damage to the eye.”
“It is crucial to diagnose and treat AMD as early as possible to prevent irreversible loss of central vision.”
It is also recommended that first-degree relatives of AMD patients monitor their eye health on a regular basis with simple non-invasive tests.
Diagnosis of AMD can be achieved with just three non-invasive tests, including visual acuity measurement , dilated retinal examination , digital fundus flourescine angiography and optical coherence tomography (OCT) of the macula.
Regular eye checks are vitally important for all.
Our Retinal Services
- Advanced Vitreo-Retinal Surgery
- Diabetic Eye Disease Clinic
- Green Retinal Lasers
- Diode Retinal Lasers
- OCT
- Digital Fundus Fluorescein Angiography
- Indocyanine Green Angiography
- Fundus Auto Fluorescence
- ANTI-VEGF Therapy Injections
- ROP Screening